You are not crazy for wondering why your head still pounds years after that blast, rollover, or training accident. Post deployment life was supposed to feel calmer, but post-TBI headaches, VA migraine VA rating traumatic brain injury claim issues can make every day feel like a fight. The administrative burden often feels heavier than the injury itself.
Maybe you are sitting in a dark room right now, trying to ride out another migraine, wondering how the VA decides what your pain is worth. You might be stuck at a 0 or 10 percent rating. Deep down, you know your headaches are doing way more damage than your current rating shows.
This guide walks you through how the VA looks at post-TBI headaches and migraines. We will look at how ratings actually work and how to build a strong traumatic brain injury claim. You will also see where many veterans get tripped up and how you can avoid those same traps.
Why Post TBI Headaches Hit So Hard For Veterans
First, you need to know this is not all in your head in the casual sense. The numbers back you up in a big way. You are relying on solid medical evidence regarding traumatic brain injuries.
The VA Office of Research and Development reports that between 2000 and 2019, almost 414,000 TBIs were documented in service members. That is a huge number of brain injuries across all branches of the military. Headaches are one of the most common lingering symptoms after those injuries, according to the VA Office of Research and Development.
Medical research backs this up consistently. One study in the National Library of Medicine found that a year after head trauma, about 18 to 22 percent of patients still had headaches. Headaches were the most common physical complaint after a TBI, which you can see at this TBI headache study.
Another large study found that people with TBIs had about a 1.5 times higher risk of migraine than those without TBI. The same research showed that those who needed hospitalization for severe TBI were even more likely to develop migraine. This is discussed in this migraine risk paper.
If it feels like almost every other veteran you know has head pain or migraine after blasts or concussions, you are not far off. VA itself has said migraine diagnoses rose by 27 percent across all service branches from 2001 to 2007. They shared that figure here: VA migraine increase report.
One deployment based study found that about 36 percent of service members who spent at least a year in Iraq had migraine symptoms. This data highlights the prevalence of tbi migraines in combat zones. VA wrote about that finding in more detail at this deployment headache study.
How VA Thinks About TBI, Migraines, And Residuals
This is where things start to feel confusing because the VA does not rate your TBI by itself in most cases. Instead, it rates what are called tbi residuals. These are the lasting symptoms caused by that original injury.
The basic rule comes from 38 CFR 4.124a, which explains that TBIs are rated based on current residual symptoms and functioning. Understanding how the VA rate is applied requires looking at the regulations. You can read the actual regulation at 38 CFR 4.124a.
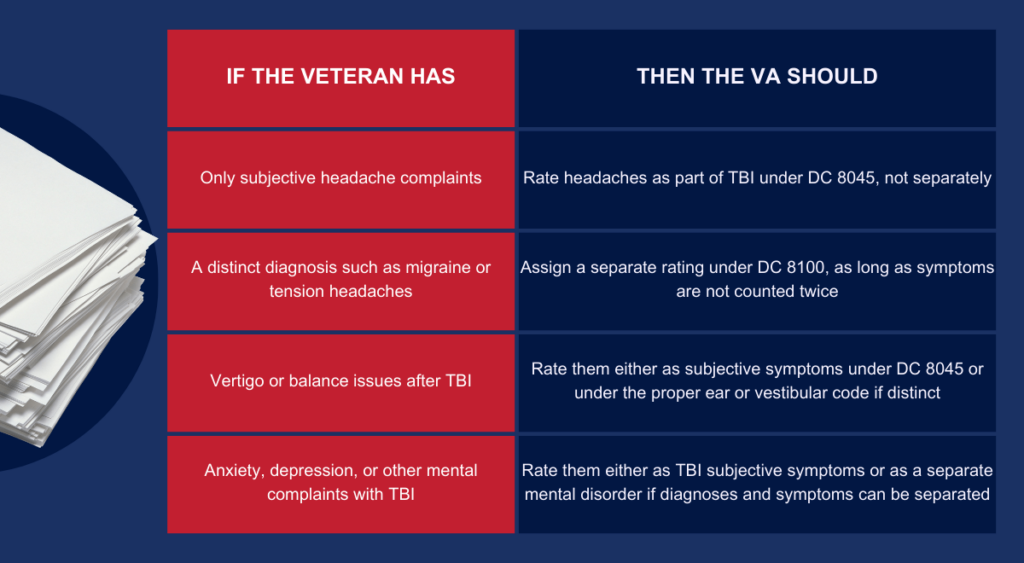
The rating for TBI residuals uses diagnostic code 8045. This covers problems with thinking, memory, judgment, behavior, and certain physical issues tied directly to the brain injury. The full table sits at DC 8045 rules.
But VA rules also say that any distinct diagnosis that can be rated under a different diagnostic code can get its own separate rating. This applies as long as the symptoms are not counted twice. This is written right into 38 CFR 4.124a.
That matters a lot for you. Migraine headaches have their own diagnostic code, DC 8100, with a separate rating scale. This allows you to potentially receive a VA disability benefit for both the TBI itself and the headaches.
How Migraines And Post Concussive Headaches Are Rated
Many veterans do not realize this, but your post-TBI headaches might deserve a rating all on their own. That is true even if you already have a TBI rating. A mild tbi can still result in severe migraine symptoms.
Diagnostic Code 8100 is used for migraine headaches, which includes many post concussive headaches after TBI. The schedule describes levels based on the frequency and impact of characteristic prostrating attacks. You can read a key decision that walks through this language at this DC 8100 case example.
It is vital to understand specific phrases used by the VA. Characteristic prostrating means the migraine forces you to stop activity and rest completely. This often involves lying down in a dark room.
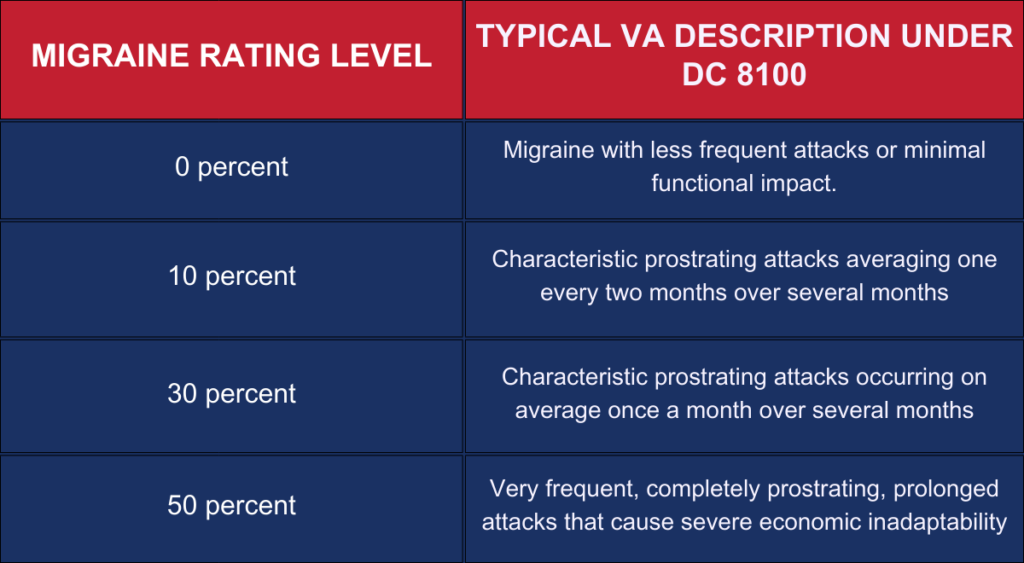
The top schedular rating under DC 8100 is 50 percent. Many veterans never reach it because their medical records and lay evidence do not fully show how disabling their headaches really are. Getting the correct disability ratings requires precise documentation.
VA training materials explain that there is a difference between basic headache complaints and a separate diagnosis. Examples include migraine, tension headaches, or post concussive headaches. Those with a distinct diagnosis can often be rated separately under DC 8100.
This is only allowed if the symptoms do not overlap with the ones already counted under DC 8045. This point shows up in VA internal guidance at DC 8045 guidance.
You can also find this in the VA manual section on neurological conditions here: M21 1 neurological section. This is good news for you if your headaches have a formal diagnosis. Your doctor must show they cause problems above and beyond your base TBI symptoms.
Toxic Exposure and Agent Orange Factors
Sometimes headaches and neurological issues are not solely from a physical blow to the head. Toxic exposure during service can also lead to similar symptoms. Veterans with agent orange exposure often report complex health issues.
The PACT Act has expanded how the VA looks at toxic wounds. If you served in the Gulf War or on certain military bases, you might have presumption for other conditions. Military base toxic exposure is becoming a larger part of the conversation regarding brain health.
Agent orange causes systemic issues that can affect the nervous system. While headaches are not always a presumptive condition for agent orange alone, the overall toxic load can complicate a TBI claim. Orange exposure creates long-term health risks that the VA is slowly acknowledging.
You should check if your service history places you near burn pits or specific zones of base toxic exposure. Exposure to chemicals on a military base toxic site can worsen existing neurological conditions. Always include this history in your disability claim.
If you have Parkinsonâs disease, which is presumptive for agent orange, this changes how your rating is calculated. The combination of a TBI and a condition like Parkinson’s can lead to a higher overall percent rating. Understanding the base toxic environments you worked in is essential for a complete file.
How TBI, Migraines, Mental Health, And Other Issues Fit Together
If you feel like your symptoms blend together, you are not alone. Many veterans deal with headaches, memory issues, mood swings, vertigo, sleep trouble, and more. These often all stem from the same original event.
VA policy accepts that the external force that caused the TBI can lead to both direct brain injury and separate conditions. These can be mental, neurologic, or physical. These may be rated apart from the base TBI residuals if they have clear diagnoses.
This is recognized under 38 CFR 4.124a, DC 8045, and 38 CFR 3.303 for service connection rules. You can review the texts at DC 8045 text and 38 CFR 3.303. Properly separating these allows for accurate va claims.
VA has also given rating staff more detailed guidance on how to handle overlapping TBI and mental health symptoms. This often involves looking at cognitive impairment versus emotional symptoms. The M21 manual section for TBI claims clarifies this separation.
If an examiner can clearly separate which symptoms belong to TBI and which belong to a mental disorder, each one may get its own rating. That guidance is at M21 1 TBI section.
One more legal point that trips up a lot of veterans is pyramiding. VA rules say the same symptom cannot be counted twice under two codes. That is spelled out at 38 CFR 4.14.
The M21 manual and cases such as Esteban v. Brown talk more about how to avoid pyramiding. These resources explain how to still give fair ratings. You can explore this here: M21 pyramiding guidance and Esteban decision summary.
Secondary Conditions and Additional Claims
A severe TBI or even a mild one can cause a domino effect in your body. This often leads to a secondary condition that can be service connected. For example, sleep apnea is sometimes linked to brain injuries affecting central respiratory control.
If you have a TBI rating, look out for other health changes. Psychiatric disability claims, such as depression or anxiety, are common secondary claims. You must show that the TBI caused or aggravated these new conditions.
Even hearing issues can be complex. While tinnitus is common, central auditory processing disorders are TBI based. A standard hearing disability calculator might not capture the full extent of a brain-based hearing issue.
When you file for a secondary condition, you need a medical opinion linking it to the TBI. This opinion must state it is “at least as likely as not” caused by the service connected injury. This is a critical piece of evidence for VA disability benefits.
Building A Strong Post TBI Headache And Migraine Claim
So how do you move from vague complaints to a tight, well supported claim? You want to make it hard for the VA to lowball your rating. You start with the basics and stack proof for each element.
Service connection for post TBI headaches and migraines usually has three main parts. First is a current diagnosis such as TBI, post concussive headaches, or migraine. You need this in your medical records.
Second, you need proof of the in service event. This could be a blast, crash, fall, or other trauma. Third, you need a nexus link tying the current condition to the in service trauma.
Many veterans already have service connection for TBI. They are trying to raise their rating by showing how bad their headaches really are. Others are trying to add migraines as a separate service connected disability.
The Right VA Forms For TBI Headache Claims
You start the process with the standard disability form, VA Form 21 526EZ. This is the main application for disability benefits. VA explains how to use it here: VA Form 21 526EZ.
You can then use VA Form 21 4138, Statement in Support of Claim. Use this to share more details or add a personal statement about your headaches. It is also good for buddy statements from people who see what you go through.
These forms might feel boring or technical, but they are vital. Your words can be just as important as your medical notes.
Describe how headaches knock you out. Mention if they cost you jobs or force you to miss time with family. This personal testimony adds weight to your file.
Evidence That Helps Post TBI Headache Ratings
There is a simple rule of thumb for evidence. The higher your desired rating, the clearer your records need to be. You must document the number, length, and impact of your headache attacks.
Useful evidence includes items like this list.
- Neurology or primary care records with a firm migraine or post concussive headache diagnosis.
- Notes that mention aura, light or sound sensitivity, nausea, and having to lie down in a dark room.
- Employer records or personal statements showing missed work or loss of income due to headaches.
- Spouse or family statements that describe how you shut down during attacks.
- A simple headache log, kept daily for at least 30 to 60 days, tracking severity and time lost.

Most veterans are under rated because the medical notes are too vague. They might simply say “history of headaches” or “intermittent migraine.” This does not tie the condition to time missed from work.
You need to show the need to lie flat in a quiet room. You can guide your doctors to record the impact better by sharing details at every visit. Make sure they document the phrase “prostrating” if it applies.
Understanding Economic Impact, TDIU, And Headaches
You might read the 50 percent migraine rating phrase “severe economic inadaptability” and wonder what it means. Does it mean you must be fired from every job? Or that you cannot work at all?
VA regulations give a bit more context. Total Disability based on Individual Unemployability, or TDIU, is a separate benefit. It is for veterans whose service connected disabilities stop them from working full time.
The main rule set is at 38 CFR 4.16, found here: 38 CFR 4.16a. If your post TBI migraines or headaches cause you to miss a lot of work days, look into this. It applies if full time work becomes impossible.
Your case might support both a higher DC 8100 rating and TDIU. Think of it like this. DC 8100 50 percent asks whether attacks are frequent and disabling regarding stable employment.
TDIU asks whether the sum of your rated conditions prevents you from doing substantially gainful work. If headaches from your TBI keep sending you home from work early, record it. Or if you left jobs due to absence tied to migraines, note that.
Make sure this is recorded clearly in both your medical file and lay evidence. This is exactly the type of thing raters look at for severe economic impact. It directly influences your eligibility for total disability.
Calculating VA Disability Rates and Compensation
Understanding VA disability rates can be difficult. The VA uses “va math” to combine ratings. This means a 50% rating and a 30% rating do not simply equal 80%.
You might look for a disability calculator online to help estimate your combined score. Knowing your combined rating determines your monthly compensation. Higher ratings lead to significantly higher financial support.
Disabled veterans with a rating of 30% or higher also receive extra compensation for dependents. This is why getting the accurate VA disability ratings for every condition matters. Even a 10% rating for a secondary condition can bump your overall pay.
Check the current disability rates tables to see where you stand. The difference between 90% and 100% is substantial in terms of monthly compensation. Fighting for that extra rating for migraines can bridge that gap.
How TBI Headaches Compare To Other VA Ratings
VA rating rules have some common threads across different conditions. If you already have other service connected conditions, the logic might feel familiar. The VA looks for frequency, severity, and duration.
For example, if you have digestive issues from service, your case may be rated under different diagnostic codes. Each is tied to specific symptoms, just like with TBI and migraines. Veterans law applies similar principles of proof across the board.
If you ever need help with ratings outside the head injury space, these guides may help. They help you make sense of how VA thinks across different body systems. The logic remains consistent.
- A detailed look at how VA handles swallowing problems and how a va rating is decided for dysphagia.
- An explanation of how abdominal pain and inflammation are rated in this va rating guide for gastritis.
- For pancreas issues and pain, you can see how that va rating is broken down for pancreatitis.
The key idea is the same. The VA cares about how often symptoms happen. They care how intense they are and how much they affect daily life and work.
Legal Resources and Case Evaluations

Sometimes you need help with a claim. Veterans law is complex, and sometimes legal help is necessary. Many law firms offer a free case evaluation to see if they can help.
Civil personal injury cases also look hard at headaches and brain function. Injury attorneys use these facts to calculate settlement ranges. For example, you can see how serious burns might be valued in a civil injury claim guide from one firm.
If your TBI or headaches came from a crash in a different country, the process can be tangled. Law firms that handle cross border cases have their own guidance. You can read this breakdown on cross border injury claim strategies.
Even within brain injuries, lawyers watch how spinal cord or severe brain cases are handled. It shapes how judges and juries think about long term damage. You can see that style of thinking in this overview of a spinal cord injury claim or a case result for a severe traumatic brain injury.
Motorcycle wrecks are a big example of this. Even riders wearing helmets are at high risk of TBI if they go down at speed. This risk is outlined in a legal article on motorcycle crashes and brain injury.
Head injury concerns also come up in pro sports. Harvard Health has written about long term brain injury issues in NFL players. This looks a lot like what many combat veterans deal with decades after the fact.
Why mention all this here? It reminds you that your headaches are a recognized part of serious head trauma. If you are struggling, seeking a free case review from a firm specializing in va benefit law can be a smart move.
How VA Treats Multiple Evaluations And Pyramiding In TBI Headache Claims
To really understand your post-TBI headaches VA migraine VA rating traumatic brain injury claim, you need to know about pyramiding. You must know how VA handles situations where many symptoms overlap. The goal is to maximize your rating without breaking the rules.
In TBI cases, raters must review each symptom and ask two questions. First, does this belong in the main TBI residuals table under DC 8045? Second, does this symptom have a distinct diagnosis that deserves a separate code?
VA manual guidance on TBI explains that separate ratings are possible. This happens if you have both TBI residuals and a diagnosed mental or neurocognitive disorder. The examiner must be able to separate which symptoms go with each.
But if the symptoms and occupational effects cannot be teased apart, then one rating must be chosen. The VA must choose whichever gives the higher evaluation. That policy sits in detail at this M21 1 TBI policy.
The same logic is used with hearing, tinnitus, and vestibular issues after TBI. For instance, tinnitus might be rated under 38 CFR 4.87 DC 6260. Balance issues might sit under DC 8045 or a separate vestibular disorder code.
Those rating instructions sit here: 38 CFR 4.87 DC 6260. For you, this means your file should clearly separate symptoms whenever possible. You want the neurologist, psychologist, and primary doctor to be specific.
Each provider should say what belongs where. This gives raters the room to assign multiple evaluations without pyramiding. Clear medical evidence is the solution to pyramiding issues.
Common Mistakes That Sink TBI Migraine Ratings
If your rating is stuck or you keep getting lowballed, look for common errors. Chances are one of these issues is at play. The good news is they can be fixed.
- No clear migraine or headache diagnosis, only a vague history of headaches in your file.
- Medical notes mention headaches, but there is no record of time lost from work.
- There is no mention of the need to lie down or prostrate oneself.
- Your TBI residuals are rated, but no one ever requested a separate DC 8100 migraine rating.
- Doctors or examiners do not explain how headaches impact your economic life and daily function.
- Your statements talk about pain levels but never spell out how many days a month are wiped out.
The VA is supposed to apply the rules fairly. However, they can only rate what is in front of them. You must use clear language regarding your attacks.
If no one states you have prostrating attacks twice a month, raters will not guess it. You need to state that these attacks put you in a dark room for six hours. If they cause you to miss work, that must be in the file.
Long Term Health Risks That Make Proper Ratings Even More Important
Your rating is about more than money. It can affect access to treatment and your family security. It also impacts how the VA tracks long term risks for veterans with TBI.
Research on post 9/11 veterans found that mortality rates were higher than expected. Those with TBI had the greatest risk.
VA summarized it in this TBI mortality report. Another set of findings from VA research talks about how TBIs can change health decades later. They discuss how mood disorders, headaches, and sleep problems connect.
Those big picture data sets are part of why VA invests in TBI and headache care. You can read about this in VA TBI research updates. Knowing this, fighting for a fair rating is really about your health history.
You need to make sure your record matches the real long term seriousness of head injury. Your future self might need that accurate record. Your family depends on the benefits that come with proper acknowledgment.
Putting It All Together For Your Claim
If you feel overwhelmed, that makes sense. Post TBI headaches, VA migraine VA rating traumatic brain injury claim rules can feel like a foreign language. But once you break it down, there is a clear path forward.
You start by getting your diagnoses tight. Collect evidence that shows the frequency and impact of your attacks. Use the right VA forms to put that story in writing.
Study the rules at 38 CFR 4.124a for DC 8045 and DC 8100. This ensures you know exactly what the rater should be looking at. Then you push gently but firmly for your providers to document things correctly.
Guide them to use words the rating schedule cares about. Focus on “prostrating attacks,” “time lost from work,” and “severe economic impact.” That is where ratings jump from 0 or 10 to 30 or even 50 percent.
Conclusion
Your story, like so many others, may include a blast, crash, or impact that happened in a split second. This was likely followed by years of grinding headaches, blurry days, and missed moments. You did not ask for any of that, and you should not have to carry it without proper support.
Understanding how the VA looks at post-TBI headaches VA migraine VA rating traumatic brain injury claim issues puts some power back in your hands. You now know that TBI is rated by residual symptoms. You know that migraines have their own code.
You also know that overlapping conditions can be rated separately when documented the right way. This must be done under the rules in 38 CFR 4.124a, DC 8045, DC 8100, and related sections. Use this knowledge to build a cleaner file.
Gather stronger evidence and a more complete story of what you live with every week. Your pain is real, and the research backs you up. The rating schedule has room to reflect the full weight of what TBI headaches and migraines have taken from you.

