Migraines can be debilitating. Learn how to prove them to the VA and secure a high disability rating.
For many veterans, migraines are more than “just headaches.” They are chronic, disabling neurological events that disrupt work, family life, and daily functioning. Yet, far too many VA claims for migraines are denied or underrated—especially when veterans did not receive a formal diagnosis while in service.
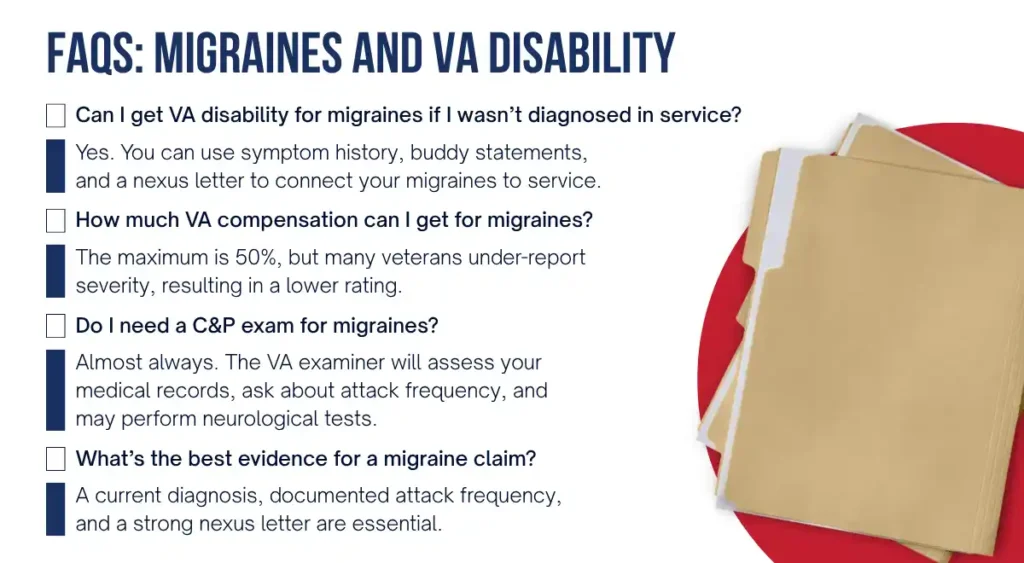
The good news: You can still win your VA disability claim for migraines, even if they weren’t documented during active duty—if you know how to provide the right medical evidence.
Why Migraines Matter in VA Disability Claims
Migraines are one of the most common conditions for which veterans seek VA disability benefits. According to the VA’s Office of Inspector General, migraines are among the top five service-connected conditions in recent years.
Veterans often experience migraines due to:
- Head trauma (TBI or concussions during service)
- Exposure to toxins or burn pits
- Stress and mental health conditions (PTSD, anxiety, or depression)
- Service-related neck and back injuries
- Medication side effects
Yet, the VA frequently denies claims when service records don’t show a diagnosis—even though migraines may develop or worsen over time.
VA Requirements for a Successful Migraine Claim
To receive VA disability benefits for migraines, veterans must establish service connection by meeting three core requirements. Each element is equally important, and missing just one often leads to claim denials or low ratings. Here’s what the VA looks for:

✅ 1. A Current Medical Diagnosis of Migraines
The VA will not grant service connection based only on self-reported headaches or vague medical history. You must have a formal diagnosis of migraines from a qualified medical provider, such as a neurologist, primary care physician, or headache specialist.
- This diagnosis should follow recognized medical criteria (e.g., International Classification of Headache Disorders, VA’s disability guidelines).
- Your provider should clearly distinguish migraines from tension headaches, cluster headaches, or sinus pain, since the VA requires specificity.
- A diagnosis also helps determine severity and frequency, which directly impacts your VA disability rating under Diagnostic Code 8100.
📌 Tip: If you haven’t received a clear diagnosis yet, it may be wise to schedule a neurological evaluation and request documentation that aligns with VA standards.
✅ 2. Evidence of an In-Service Event, Injury, or Onset of Symptoms
Even if you were never officially diagnosed with migraines during service, you can still prove service connection by showing evidence that symptoms began or were aggravated while in uniform.
This evidence may include:
- Service treatment records (STRs): Notations of repeated headaches, prescriptions for strong pain relievers, or medical visits where you complained of migraine-like symptoms.
- Sick call notes or duty limitations: Records showing time off duty or reduced responsibilities due to head pain, nausea, or sensitivity to light/noise.
- Lay statements: Written testimony from fellow service members, family, or friends describing your headaches during or immediately after service.
- Deployment or environmental exposure evidence: Proof of traumatic brain injury (TBI), exposure to burn pits, chemical toxins, or blast events that often trigger chronic migraines later.
📌 Tip: Even a single documented head injury or repeated complaints of severe headaches in service can be enough to satisfy this requirement when paired with a strong medical nexus.
✅ 3. A Medical Nexus Linking Migraines to Service (or a Secondary Condition)
The nexus is the bridge between your current diagnosis and your military service. Without it, the VA will almost always deny your claim.
- A nexus letter from a qualified, independent medical provider carries significant weight because it uses VA-compliant language like “at least as likely as not” to establish service connection.
- The provider should explain the medical rationale, citing both your records and credible research, to show how your migraines are linked to:
- An in-service injury (e.g., concussion, head trauma, blast exposure)
- Service-related conditions (e.g., PTSD, cervical spine injuries, TBI)
- Medications prescribed for other service-connected disabilities that may trigger migraines
Example of a strong nexus statement:
“It is at least as likely as not that the veteran’s migraine condition is a result of his documented TBI sustained during active service, given the well-established medical association between head trauma and post-traumatic migraines.”
📌 Tip: A well-drafted nexus letter often makes the difference between a denial and an approval. Veterans who file without one risk leaving their claims incomplete.

✅ Bottom Line:
To win a VA claim for migraines, you need all three pieces—diagnosis, evidence of in-service symptoms or events, and a medical nexus. Think of it as a three-legged stool: if one leg is missing, the claim collapses.
Proving Migraines Without an In-Service Diagnosis
One of the biggest hurdles veterans face is lack of a migraine diagnosis in service records. Here’s how to overcome it:
1. Show Symptom History and Continuity. Even without a formal diagnosis, you can demonstrate that migraine symptoms began in service and continued after discharge. Use:
- Service treatment notes (complaints of headaches, light sensitivity, nausea)
- Buddy statements from fellow service members or family describing your headaches during/after service
- Personal statements (VA Form 21-4138) detailing frequency, severity, and functional impact
2. Highlight Secondary Service Connection
Migraines are often secondary to another service-connected condition. For example:
- PTSD → stress-induced migraines
- TBI → post-traumatic migraines
- Cervical spine injury → tension headaches evolving into migraines
- Hypertension medications → side effects triggering migraines
If you already have one of these conditions service-connected, you can strengthen your migraine claim with a secondary nexus letter.
3. Secure a Strong Medical Nexus
A VA-compliant nexus letter is often the deciding factor. The provider must:
- Use VA’s standard of proof (“at least as likely as not”)
- Cite medical literature linking your service event or condition to migraines
- Provide a clear medical rationale that bridges gaps in your service records
Example nexus statement:
“It is at least as likely as not that the veteran’s current migraine condition is secondary to his service-connected PTSD, given the well-documented link between chronic stress, SSRIs, and migraine onset.”
The VA uses Diagnostic Code 8100 to assign ratings:
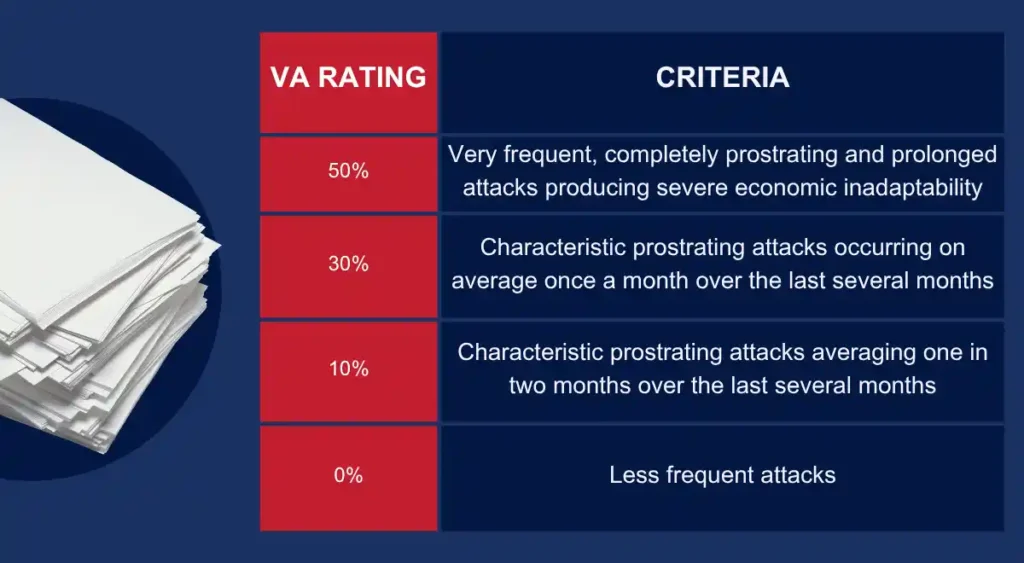
Key tip: The VA focuses on the frequency and severity of “prostrating attacks” (episodes that force you to lie down and stop all activity). Documenting how often migraines prevent you from working or functioning normally is critical to securing the highest rating possible.
Common Mistakes That Lead to Denials in Migraine VA Claims
Many veterans with severe, life-disrupting migraines are denied VA disability benefits—not because their condition isn’t real, but because their claim is missing critical evidence. Understanding the most common pitfalls can help you avoid unnecessary delays, denials, and appeals.
❌ Filing With Headache Symptoms Only, Not a Formal Diagnosis
The VA does not grant disability benefits for “headaches” alone. A formal medical diagnosis of migraines is required. Veterans sometimes submit claims based only on self-reported pain or outdated service treatment notes, but without a doctor’s confirmation, the VA cannot rate the condition under Diagnostic Code 8100.
👉 Tip: Schedule an evaluation with a neurologist or other qualified provider. Make sure “migraines” is explicitly listed in your medical records, not just “headaches.”
❌ Failing to Document Functional Impact
The VA rates migraines not just on their existence, but on how much they impair your daily life and ability to work. Veterans often miss out on higher ratings because they don’t provide evidence of functional limitations, such as:
- Time missed from work or reduced productivity
- ER visits or urgent care for migraine attacks
- Being bedridden during prostrating episodes
- Impact on daily functioning (driving, caring for family, handling bright light or loud noise)
👉 Tip: Keep a migraine log or journal documenting attack frequency, duration, and severity. Share this with your doctor so it becomes part of your official medical record.
❌ Not Connecting Migraines to PTSD, TBI, or Other Conditions
Many migraines are secondary to service-connected conditions, but veterans sometimes fail to make the connection. Migraines may be triggered or worsened by:
- Traumatic Brain Injury (TBI) – blast exposure, concussions, or head trauma
- Post-Traumatic Stress Disorder (PTSD) – stress, sleep disruption, or medications
- Cervical spine conditions or musculoskeletal injuries – nerve irritation or chronic pain leading to migraines
- Service-connected medications – certain blood pressure meds, antidepressants, or pain relievers
👉 Tip: If migraines began after you were diagnosed or treated for another service-connected condition, highlight that connection and secure a medical opinion that explains it.
❌ Submitting a Claim Without a Medical Nexus Letter
Even with a diagnosis and strong medical history, the VA often denies claims if there is no explicit nexus statement connecting migraines to military service. A VA-compliant nexus letter from an independent medical provider is often the “make-or-break” factor.
- The letter must use language like “at least as likely as not” to meet VA’s legal threshold.
- It should reference your service treatment records, current medical evidence, and established research.
- Without this, the VA may dismiss your migraines as “unrelated” or “not service-connected.”
👉 Tip: Work with a provider experienced in VA disability standards—many civilian doctors don’t understand the specific language required.
✅ Bottom Line:
Avoiding these mistakes can dramatically improve your chances of winning your migraine VA claim. The difference between a denial and a high rating often comes down to whether you provide:
- A clear diagnosis,
- Documentation of impact,
- A recognized secondary connection, and
- A strong nexus letter.
Why Work with Vet Claim Solutions?
Navigating VA claims for migraines is complex and frustrating, especially without in-service documentation. That’s where Vet Claim Solutions helps.
We provide:
- Independent medical nexus letters tailored for VA standards
- Medical records reviews to identify overlooked evidence
- DBQs (Disability Benefits Questionnaires) that clearly document severity
- Specialist medical opinions linking migraines to PTSD, TBI, or medications
Our veteran-owned, veteran-centered mission is simple:
👉 To deliver the strongest medical evidence so you can secure the benefits you earned.
Take the Next Step
Migraines are more than headaches—they are life-altering conditions that deserve fair recognition by the VA. Don’t let missing in-service records or weak evidence stand in your way.
📞 Contact Vet Claim Solutions today to get started with a medical nexus letter or records review from a trusted provider who knows what the VA needs to see.


