Chronic Fatigue Syndrome (CFS / ME) is disabling for many veterans. Yet CFS claims are commonly denied because the condition is symptom-based, often lacks a single confirmatory lab test, and can appear years after service. A strategically documented claim — using medical records, symptom logs, the VA DBQ, and a strong nexus letter — is how you turn symptoms into an approved VA rating. (We’ll show exactly what evidence to collect and how the VA evaluates it.)
How to Document Symptoms, Prove Service Connection, and Win Benefits
To win a VA claim for Chronic Fatigue Syndrome (CFS, also called ME/CFS), you need a current, VA-compatible diagnosis, medical evidence showing symptoms and functional loss, and a medical nexus linking CFS to your military service (or to a service-connected condition). Gulf War veterans may qualify under presumptive rules in 38 C.F.R. §3.317 — and the VA evaluates CFS under Diagnostic Code 6354 with ratings that range from 10% up to 100% depending on severity and incapacitating episodes.

Why this matters
Chronic Fatigue Syndrome (CFS / ME) is disabling for many veterans. Yet CFS claims are commonly denied because the condition is symptom-based, often lacks a single confirmatory lab test, and can appear years after service. A strategically documented claim — using medical records, symptom logs, the VA DBQ, and a strong nexus letter — is how you turn symptoms into an approved VA rating. (We’ll show exactly what evidence to collect and how the VA evaluates it.)
What is CFS / ME
CFS — also called Myalgic Encephalomyelitis (ME/CFS) — is a chronic, multisystem illness characterized by debilitating fatigue not relieved by rest, post-exertional malaise, cognitive problems, sleep disturbance, and other symptoms that significantly reduce daily functioning. There’s no single lab test; diagnosis is clinical, based on symptom patterns and excluding other causes. For clinical diagnostic guidance see CDC/NAM criteria.
VA’s legal/medical framework for CFS (the essentials)
1) VA diagnostic standard (what the VA requires)
For VA purposes a CFS diagnosis requires:
- New onset of debilitating fatigue reducing daily activity to less than 50% of pre-illness level for at least 6 months, and
- Exclusion of other medical causes, and
- Six or more specified symptoms (examples include post-exertional malaise, sore throat, tender lymph nodes, muscle pain, headaches, cognitive impairment).
(These VA-specific elements come from 38 C.F.R. §4.88a and the VA’s Chronic Fatigue Syndrome DBQ.)
2) Gulf War / Southwest Asia presumptive rules
If you are a Gulf War / Southwest Asia theater veteran, CFS may be presumptively service-connected under 38 C.F.R §3.317 when it manifests within the regulatory period — meaning you may not have to prove direct causation if your condition meets the manifest/period requirements. Check the VA Gulf War illnesses page and 38 C.F.R. §3.317 for eligibility details.
3) How the VA rates CFS (Diagnostic Code 6354)
CFS is evaluated under DC 6354. Ratings are based on symptom severity, frequency, and functional impact (examples below). Ratings commonly seen: 10%, 20%, 40%, 60%, 100%, depending on whether symptoms cause intermittent incapacitation, continuous significant activity reduction, or near-total loss of routine activities. (See the schedule language in §4.88b/DC 6354.)
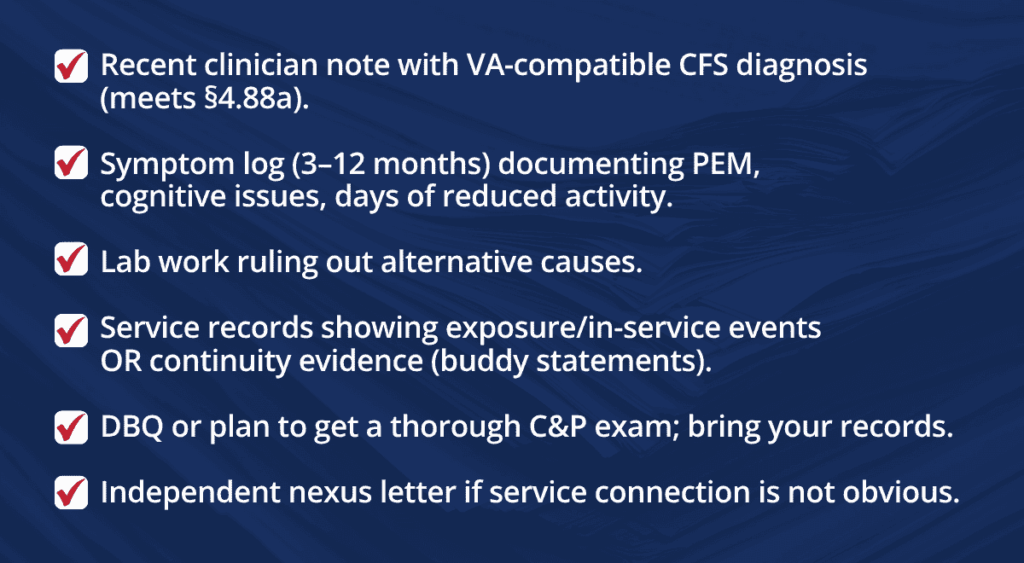
What evidence the VA needs (actionable checklist)
To maximize approval odds and the correct rating, collect and submit all of the following:
✔ A current, documented medical diagnosis of CFS in VA or private records using the VA criteria (duration, symptom list, exclusion of other causes).
✔ Complete medical records showing onset and course (service records, post-service treatment notes, ER visits, specialty consults).
✔ DBQ for CFS — the VA’s disability benefits questionnaire for CFS should be completed by an examiner during the C&P exam and will be used to evaluate frequency, severity, duration, and functional impact.
✔ Symptom journal / activity log showing day-to-day limitations, post-exertional malaise episodes, and how routine tasks have dropped below 50% of pre-illness levels. (See VA diagnostic threshold about <50% activity.)
✔ Objective test results and labs used to rule out other causes (thyroid, anemia, autoimmune, infectious workup). The VA requires exclusion of other clinical conditions.
✔ Buddy and family statements describing continuity of symptoms (helps when service records are sparse).
✔ Medication and treatment history documenting physician-prescribed therapies, hospitalizations, bed rest orders, or prolonged incapacity.
✔ A clear, VA-style nexus letter or medical opinion tying CFS to service (or to an already service-connected condition). See the nexus section below.
How the VA assigns ratings for CFS: Build a claim that wins (process & tips)
Step 1 — Get the right diagnosis (and document exclusion)
- See a clinician familiar with ME/CFS (primary care, infectious disease, or specialty clinic) and ask them to apply VA-compatible diagnostic criteria (symptom duration ≥6 months, fatigue severity, 6+ supporting symptoms, and exclusion of other causes). Cite CDC/NAM diagnostic criteria as needed during evaluation.
Step 2 — Record daily function & flare patterns. Keep a daily log for 3–6 months: hours in bed, days missed from work, periods of severe PEM (post-exertional malaise), cognitive lapses, and activities you can no longer do or do less than 50% of prior capacity. This evidence directly maps to DC 6354 criteria.
Step 3 — Use the CFS DBQ and prepare for the C&P
- The VA examiner will complete the DBQ for CFS; bringing your symptom log, medical records, and a concise summary helps the examiner and improves exam quality. The VA DBQ outlines specific questions the rater will use, so align your evidence with it.
Step 4 — Get a focused medical nexus letter when needed
- If service records do not clearly show onset, a qualified provider should prepare a nexus letter stating whether it is “at least as likely as not” (50%+ probability) that CFS is related to service or to a service-connected condition (secondary). The M21-1 and VA medical opinion guidance emphasize clear probability language and reasoned rationale.
Suggested nexus sentence (example):
“After review of the veteran’s records and history, it is at least as likely as not that the veteran’s chronic fatigue syndrome began during/within X months of [service event] and has persisted since service, producing the documented reduction in daily activities.”
Step 5 — If you’re a Gulf War veteran, check presumptive rules
- Gulf War veterans may qualify for presumptive service connection for CFS if the condition manifested during service in the Southwest Asia theater or within the regulatory timeframes under 38 C.F.R. §3.317 — which changes require checking VA guidance and case law. If eligible, presumptive means you generally do not need the same level of causation proof. Always verify current effective dates and rules on VA.gov.
Common Reasons CFS Claims Are Denied (and How to Avoid Them)
Many veterans with Chronic Fatigue Syndrome (CFS) meet VA’s disability criteria but still receive denials or low ratings because of avoidable gaps in their evidence. Understanding the most common pitfalls can help you prepare a stronger claim from the start.
No Formal Diagnosis
The VA requires a current, medical diagnosis that meets its regulatory definition of CFS under 38 C.F.R. §4.88a.
- Self-reported fatigue, “exhaustion,” or a doctor’s note that doesn’t use VA’s criteria isn’t enough.
Examiners must rule out other causes (thyroid disease, anemia, sleep apnea, depression, etc.) before diagnosing CFS.
How to avoid this:
✔ See a provider familiar with VA’s diagnostic standards.
✔ Make sure your records clearly document symptom duration (6+ months), reduction of activity levels (≤50%), and the required supporting symptoms.
✔ If needed, request that your provider fill out the CFS Disability Benefits Questionnaire (DBQ).
No Continuity or Onset Evidence
Even with a diagnosis, the VA often denies claims if there’s no evidence linking CFS symptoms back to service.
- Service treatment records (STRs) may not document fatigue complaints.
- Gaps in medical treatment history can make it appear the condition developed later, not during or soon after service.
How to avoid this:
✔ Submit lay statements from family, friends, or fellow service members who witnessed your fatigue and functional decline after service.
✔ Highlight any STRs, deployment records, or post-deployment health assessments that mention fatigue, sleep issues, or unexplained illness.
✔ Provide private treatment records to fill in gaps between service and present day.
No Nexus (Medical Connection)
One of the most frequent reasons for denial is lack of a medical nexus opinion. The VA needs a clinician to state, in clear terms, that your CFS is “at least as likely as not” related to service or to another service-connected condition.
- Without this, even a strong claim with diagnosis and records can be denied.
How to avoid this:
✔ Obtain a nexus letter from an independent medical provider experienced in VA claims.
✔ Ensure the letter uses VA-accepted language and explains the medical reasoning, not just conclusions.
✔ For Gulf War veterans, point to presumptive service connection rules if applicable — but still strengthen your case with medical opinion.
C&P Exam Under-Capture
Even with strong evidence, a poorly documented Compensation & Pension (C&P) exam can sink a claim.
- Many veterans report that examiners understate symptoms, omit flare-ups, or fail to capture functional limitations.
- The VA heavily relies on the C&P exam report when rating claims.
How to avoid this:
✔ Bring your symptom journal, activity logs, and treatment records to the exam.
✔ Politely ask the examiner to record frequency, severity, and incapacitating episodes (e.g., physician-prescribed bed rest).
✔ After the exam, request a copy of your C&P report and check for accuracy. If errors exist, submit a written statement correcting the record.
Bottom line: Most CFS claim denials boil down to missing documentation, missing nexus, or incomplete C&P capture. By proactively addressing these issues, you significantly increase your chances of approval — and of receiving the rating that truly reflects your disability.

Secondary service connection & common comorbidities
CFS can be secondary to other service-connected conditions (for example, PTSD, TBI, or chronic infections). To get a secondary service connection you must show: (1) a service-connected primary condition, (2) a current diagnosis of CFS, and (3) a nexus linking the primary condition to CFS. A properly drafted nexus letter is often decisive in these cases.
What to expect at the C&P exam
- The examiner will ask about onset, progression, duration, pattern of PEM, how CFS affects ADLs, and prescriptions for bed rest. They will complete the CFS DBQ. Bring copies of your symptom journal, recent notes, and any lay statements. The quality of the C&P exam record heavily influences the rating.
If you were denied — next steps
- Carefully read the denial to identify whether the deficiency was diagnosis, nexus, or severity.
- Submit new and material evidence (e.g., nexus letter, new medical records) to reopen the claim or file a supplemental claim/appeal. The VA’s duty to assist may require additional exams or opinions.
Consider representation from an accredited VA claims attorney or veteran organization — and consider an independent expert opinion from a clinician experienced with ME/CFS and VA standards.
Practical checklist (what to assemble before filing)
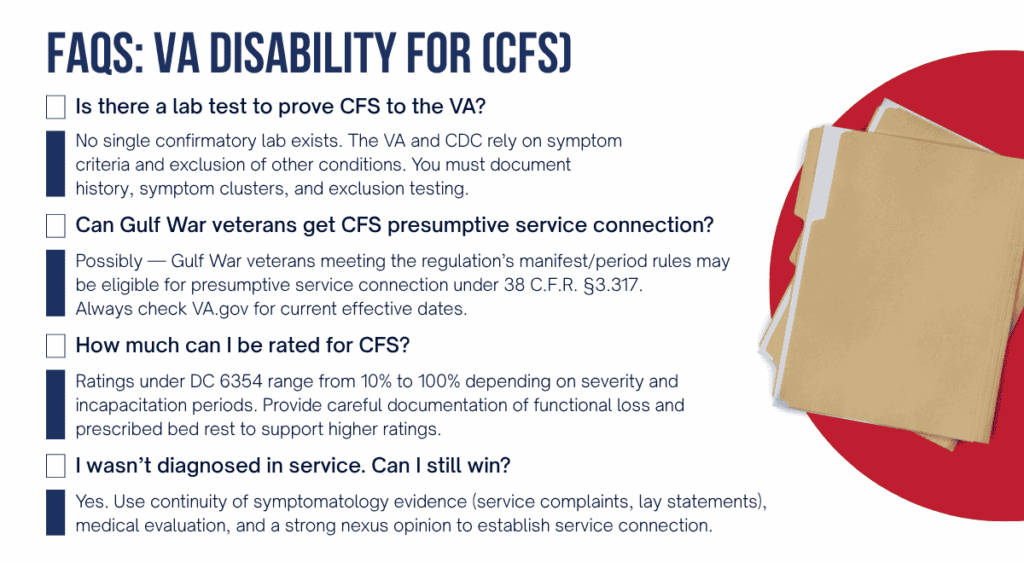
FAQs (short answers)
Why veterans choose Vet Claim Solutions
At Vet Claim Solutions we specialize in VA-ready medical evidence for complex claims like CFS:
- Independent nexus letters tailored to VA standards.
- DBQ assistance and C&P prep so your exam captures the disability accurately.
- Medical records review to identify gaps and generate supporting evidence (labs, exclusion testing, continuity documentation).
If your CFS claim was denied or you need help building a first-time claim, our clinicians and case specialists help you produce the medical evidence the VA expects.