You are not crazy for feeling like your back, legs, or feet are holding you hostage. Radiculopathy and sciatica can wreck your sleep, your mood, your work, and even simple things like walking across a room. If you are a veteran dealing with that constant nerve pain, you are also stuck dealing with VA forms, medical language, and confusing rating rules.
That is where understanding VA radiculopathy rating VA sciatica claim nerve pain veteran benefits becomes so important. If your spine, discs, or nerves were damaged in service, you deserve a fair rating and steady support. You should not have to fight this alone or feel like you are starting from scratch every time you file a va disability claim.
You might feel like the VA is speaking a foreign language while you are just trying to explain that your legs go numb. I get that. In this guide, you will see how the va rates actually work, what evidence really matters, and how radiculopathy and sciatica fit into your full benefits picture.
What Radiculopathy And Sciatica Really Are For VA Purposes
Let’s keep this simple. Radiculopathy happens when a spinal nerve root gets pinched or irritated. That nerve then starts to complain down the line, sending pain, tingling, numbness, or muscle weakness into your arms or legs.
If the nerve affected runs from your low back through your butt, thigh, and into your lower leg and foot, that is the sciatic nerve. Sciatica va claims are common because sciatica is what most people call nerve pain down the back of the leg. According to the Mayo Clinic, sciatica usually comes from a herniated disc, a bone growth, or spinal stenosis pressing on that nerve.
This is not just a civilian issue. A 2024 study showed that veterans report lower back pain at an average age of only 35. That is years earlier than non service members. That is what heavy rucks, bad landings, humvee rides, and repetitive training during military service will do.
Why Veterans Have So Much Nerve Pain In The Spine
You already know the answer, because you lived it. Repeated ruck marches and hard impacts pound the spine. Vehicle vibrations and fast rope insertions add to the cumulative trauma.
The VA Annual Benefits Report points out that sciatic nerve conditions affect veterans across all ages. That includes vets with direct spinal injuries and those with years of repetitive strain causing degenerative disc disease. Over time, a degenerative disc can bulge and press directly on the nerve roots.
Another report from the National Institutes of Health found that veterans are more likely than nonveterans to report back pain with sciatica. It also noted that severe pain was much more common in veterans who already had back pain or a diagnosed disc disease.
How The VA Sees Nerve Pain: Paralysis, Neuritis, Neuralgia
The VA likes labels. With nerve problems, it often breaks them into three groups. Paralysis, neuritis, and neuralgia.
Under 38 CFR § 4.124a, these labels are tied to specific diagnostic codes. The sciatic nerve uses codes 8520 for paralysis, 8620 for neuritis, and 8720 for neuralgia.
Here is what that means in real life, without medical school.
- Paralysis: Major loss of function, serious weakness, foot drop, or loss of motion.
- Neuritis: Pain plus sensory loss, possible weakness, dull or dead feeling, often rated as neuritis.
- Neuralgia: Pain focused along the nerve, usually burning or sharp, maybe without big weakness.
The more your symptoms match severe paralysis or serious neuritis, the higher your potential va rating. If your main problem is pain with minor numbness, VA may lean toward a lower level VA disability rating.

Where Your Radiculopathy Starts Matters
The VA rating schedule groups nerve problems based on which part of your spine is involved. It looks at the cervical (neck), thoracic (mid back), or lumbar (low back) regions. This helps determine if you have lumbar radiculopathy or another form.
Cervical Radiculopathy (Neck To Shoulder And Arm)
Cervical radiculopathy starts in the neck but causes pain or weakness in the shoulder, arm, or hand. According to research, less than one percent of people in the general population have this condition. In the military world, those numbers often feel higher, given airborne operations and repeated impact.
The va rates cervical radiculopathy with diagnostic codes 8510, 8610, and 8710. These codes cover the upper radicular group, which feeds your shoulder and elbow muscles. Severe cases can lead to muscular atrophy in the arms.
VA also looks at whether your issue is more like paralysis, neuritis, or neuralgia. Stronger loss of motion or function can reach higher percentages than “just numb fingers.”
Thoracic Radiculopathy (Mid Back)
Thoracic radiculopathy is less common, but it happens. Pain might wrap around your ribs or chest from mid back issues. This medical condition can sometimes be mistaken for other internal issues.
The VA often rates this under diagnostic code 5238, which covers thoracolumbar spine conditions. That can include spinal stenosis or disc problems in the mid region.
Your rating can be tied to both range of motion of the spine and any nerve symptoms. So you may have separate ratings, one for the spine structure and one for radiculopathy va, if it is clearly documented.

Lumbar Radiculopathy And Sciatica (Low Back To Leg)
For many vets, this is the big one. Pain shooting down the leg or numbness along the back of the thigh is debilitating. Foot weakness or drop is a common sign of lumbar radiculopathy.
Under the CFR 38, Part 4, VA Schedule of Ratings, radiculopathy that starts in the low back and runs into the leg is often linked to the sciatic nerve. For the sciatic nerve, VA uses codes 8520, 8620, and 8720. This is the core of a sciatica va rating.
Again, higher levels come with clear evidence of foot drop, little to no movement below the knee, or very limited functionality. The VA rating schedule for the sciatic nerve sets the percentages for different levels of impairment.
How VA Radiculopathy Rating VA Sciatica Claim Nerve Pain Veteran Benefits Are Decided
Now let’s tie this all together. The VA looks at both where your nerve problem starts and how bad it is. That drives your VA radiculopathy rating VA sciatica claim nerve pain veteran benefits.
For diseases of the peripheral nerves, VA follows updated guidance on diseases of the peripheral nerves. That document explains how VA weighs motor loss, sensory changes, pain, reflex changes, and overall function.
The rating schedule can sound like a legal script, but the heart of it is simple. The va disability system assigns percentages from mild symptoms around 10 percent, all the way up to 80 percent for severe sciatic nerve involvement. Ratings increase when there is a severe loss of use.
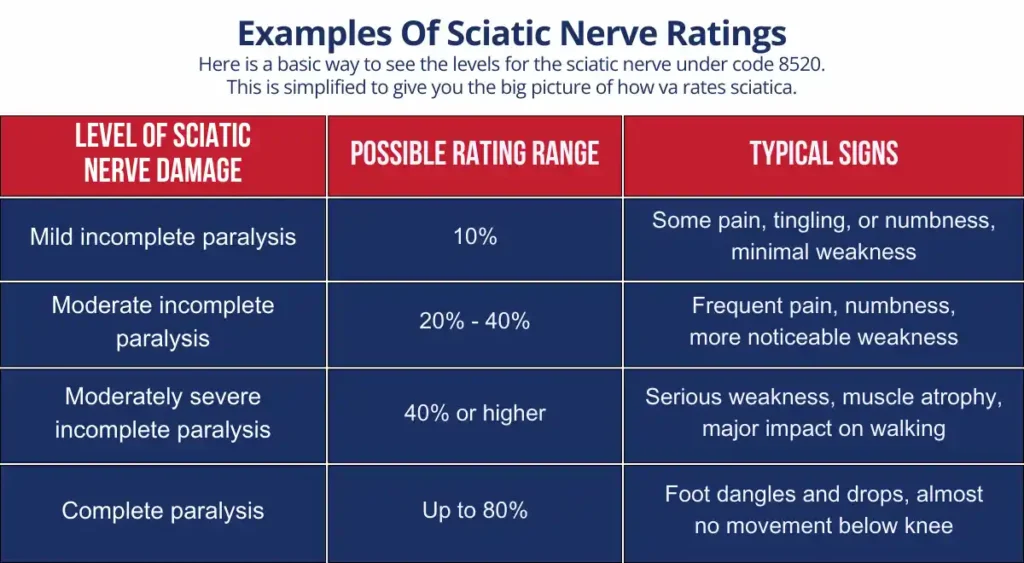
That 80 percent level is drawn from the rule that defines complete sciatic nerve paralysis. Foot drop and very weak movement below the knee are red flags the VA looks for. Anything below complete paralysis falls into an incomplete category, such as incomplete severe paralysis or incomplete severe findings.
Loss Of Use Ratings For Severe Nerve Damage
Some veterans do not just have pain. They lose almost all function of a hand or foot. That is where loss of use comes in, often placing you in a severe category.
Under §4.63, loss of use is defined as having function so poor that an amputation with a prosthetic would work as well. It is a brutal standard, but it is powerful for ratings.
If your radiculopathy or sciatica has led to near total loss of movement or sensation, that section may apply. That can drive much higher VA ratings and trigger special monthly compensation.
Service Connection For Radiculopathy And Sciatica
Your rating is one piece. First you have to win service connection. There are several ways this can happen, and you may fit more than one.
Direct Service Connection
This applies when you can point to events or injuries on active duty. Maybe you hurt your back during a training jump. Maybe years of carrying heavy loads wrecked your discs, leading to an eventual VA claim.
To win a direct service connection claim, you usually need three parts. A current diagnosis of radiculopathy or sciatica. An in service event or pattern of stress.
Finally, you need a medical link, or nexus, tying them together. That nexus letter can be from a private doctor, a VA clinician, or an outside specialist. They need to say your current nerve issues are at least as likely as not caused by service.

Secondary Service Connection
Many vets already have a service connected low back strain or spinal condition. Radiculopathy can develop years later as discs wear down and start pressing nerves. This is known as a secondary condition.
In those cases, your radiculopathy or sciatica can be rated as secondary to your main spine condition. This is where your existing rating helps. You show the primary condition, then you show that nerve symptoms began or got much worse because of it.
Sometimes, other injuries cause back problems. For example, if your knee fails, causing you to walk with a limp, that alters your gait. Over time, that awkward walking pattern can damage your spine, allowing you to file for secondary service connection.
Again, a strong medical opinion matters here. A provider should explain how the spinal problem or secondary service issue led to nerve root compression. They must detail how that compression now causes pain, numbness, or weakness.
Presumptive Service Connection In Special Cases
Most nerve claims need direct or secondary proof, but there are special presumptions too. For example, peripheral neuropathy, including sciatic neuropathy, can be treated as presumptive for veterans who were POWs for more than 30 days.
In those situations, VA does not ask you to fully prove the service cause in the usual way. They accept that this group has known patterns of damage and apply a shortcut to connection.
There are also other presumptive categories, such as for certain toxic exposures. So your service history details are very important to list out clearly in your claim.
How The VA Combines Spine Ratings And Radiculopathy Ratings
It often surprises vets that the spine and the nerves get looked at as separate items. That can actually work in your favor regarding va claims.
VA may rate your back or neck under spine codes that focus on motion loss. Then it may rate each affected nerve group on its own, using CFR 38, Part 4 for peripheral nerves. You could have ratings for both sides of your body if you experience bilateral symptoms.
Once all those percentages are assigned, they get run through the VA combined ratings table. You can use a VA disability rating calculator to see where your ratings land in a flat combined rating. The bilateral factor can boost your overall score if you have disabilities affecting both arms or both legs.

Why “Mild” And “Moderate” Language Matters
A small word in your records can cost you a lot of money. VA raters read every “mild,” “moderate,” or “severe” note and plug those into the schedule.
The radiculopathy criteria, which can range from mild 10 percent to much higher, are sensitive to this language. If your daily reality looks worse than the notes in your chart, your percent va rating may come out low.
This is one big reason to be honest and specific with your provider. If your leg gives out three times a week, say that. If your foot is numb most of the day, say that, too.
How Your Nerve Pain Impacts Your Veteran Benefits As A Whole
Nerve pain does not stop at one percentage. It affects how you walk, work, sleep, drive, parent, and live. That spillover shows up in your overall disability benefit picture.
As your combined rating rises, your financial compensation increases. That jump is larger once your combined rating crosses 30 percent and you have dependents. The benefits rating system is designed to account for family support needs.
There are other va disability benefits that become more reachable as well. Better access to care, more support programs, and help with long term planning. Even a single individual condition can unlock these doors if rated highly enough.
TDIU For Veterans Who Cannot Work
If your nerve pain, in combination with other conditions, keeps you from holding steady work, there is another door. Veterans with a combined rating of 70 percent or more can qualify for Total Disability Individual Unemployability.
TDIU pays at the 100 percent level even if your formal combined rating is lower. The question is whether your service connected issues prevent gainful work, given your background and skills.
Severe radiculopathy or sciatica often fits into this, especially if standing, walking, or sitting long blocks of time are a struggle. Severe symptoms that interrupt focus or require frequent rest breaks support this type of claim.

Other Types Of Support And Veteran Benefits
Your rating and TDIU are big, but there is more out there. For example, Aid and Attendance can help veterans who need daily help with basic tasks. This is often an overlooked disability benefits component.
You can learn about extra veteran benefits through Aid and Attendance if your limitations are serious. These programs may support in home care or assisted living needs.
Sometimes benefits overlap with your family life in quiet ways too. Simple moments at home matter a lot more when pain is constant. You may see guides on things like creative ways to enjoy holidays or special days at home, including pieces that mention veteran benefits in a home setting such as celebrations that respect your limits.
Evidence You Need For A Strong Radiculopathy Or Sciatica Claim
Your pain is real. The VA still wants paperwork. You can fight smarter by knowing what proof matters most.
Medical Evidence That Carries Weight
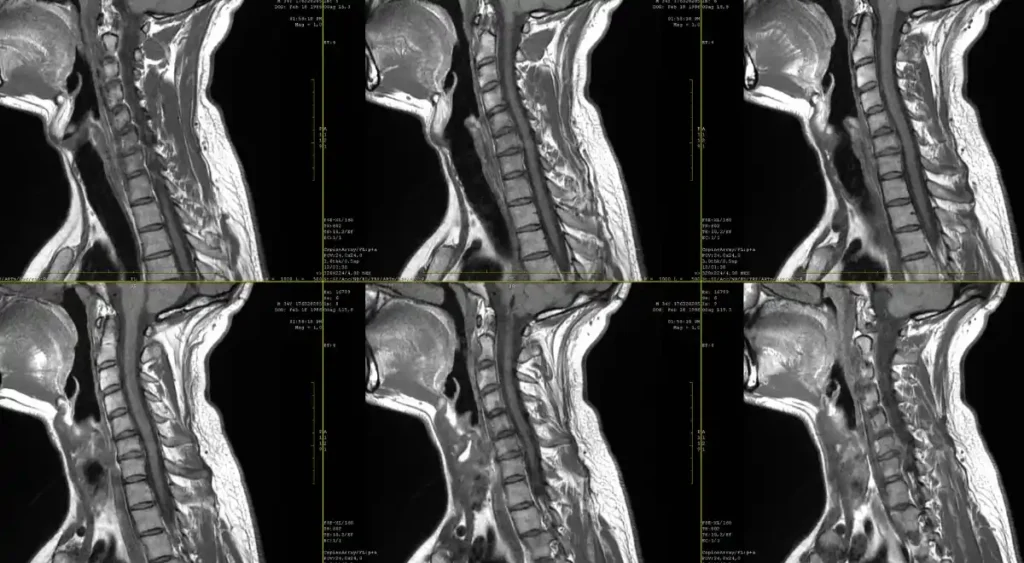
VA loves objective findings. Imaging. EMG tests. Measured strength grades. Reflex checks.
Here are some useful types of evidence you can collect.
- Recent MRI or CT scan of the spine showing disc bulges, stenosis, or bone growth.
- EMG or nerve conduction studies confirming nerve root irritation or damage.
- Neurology or orthopedic notes that describe strength loss, numb areas, or gait issues.
- Primary care notes describing sciatica or nerve pain with frequency and severity.
The VA rates radiculopathy under 38 CFR § 4.124a, Diseases of the Peripheral Nerves, using diagnostic codes 8510 through 8730 depending on which nerve is affected. So you want your medical records to clearly say which nerve root or nerve group is involved. The rates sciatica requires differ slightly from other nerves, so precision helps.

Lay Evidence: Your Story On Paper
Do not underestimate your own words. Your daily story can connect the dots the chart misses.
You can write a statement that explains when symptoms began, what movements set them off, and how they affect work and life. Friends, spouses, or co workers can submit statements too, especially if they have seen you fall, lose balance, or stop doing certain tasks.
This type of evidence shows frequency and real impact. VA raters can use it to back up higher disability ratings where the medical file may be thin on details.
How To File A VA Radiculopathy Or Sciatica Claim
You have a right to file a claim if you believe your nerve pain is service connected. You also have more than one way to get it done.
Filing Time Options
You can start early or file later. Many service members choose to file a pre discharge claim.
You may be able to file up to 180 days before your discharge. Or you can go the postservice claim route at any time after separation.
Starting early helps your case, since your medical evidence and service details are fresh. It avoids long gaps in your record which can complicate VA disability ratings later.
Ways To File Your Claim
You can file your VA disability claim online through VA’s portal. Many veterans find this the fastest route.
If you prefer paper, you can also file by mail, by fax, or in person at a VA regional office. If you choose something other than online filing, you will need to download and complete VA Form 21-526EZ.
To start the process at any point, you can grab VA Form 21-526EZ and fill it out with as much detail as possible. List your symptoms, your dates, and every related treatment center you remember.
What To Expect At A C&P Exam For Nerve Pain
A Compensation and Pension exam can feel stressful, especially if you fear not being believed. It helps to know what is coming.
In a typical radiculopathy or sciatica exam, the examiner may ask you to walk, sit, bend, and lift your legs in different ways. They will test your strength against resistance. They may use a pin or soft tool to check where you feel or do not feel sensation.
Be honest. If something hurts, say so. If you cannot repeat a movement, say why. Do not push yourself beyond what you can really do, as that only hides your limitations from the person rating your condition.
Sometimes, they may check for poor blood circulation or vascular issues to rule them out. Poor blood flow can mimic nerve pain, so distinguishing between the two is vital for an accurate va rate. Ensure you describe the specific electrical or burning nature of nerve pain.
Living With Nerve Pain While You Fight For A Fair Rating
There is the claim, and then there is your daily reality. Sciatica and radiculopathy can grind down your patience and hope if they are not treated and managed.
You may already know some of these strategies. Light stretching, controlled exercise, careful pacing, and physical therapy. The guides on easing sciatic nerve pain cover a number of simple approaches you can test with your provider.
If your nerve pain is chronic and severe, there are also medical treatments to discuss with your team. Some options, including medication strategies, are described in resources about nerve pain and in deeper looks at drugs that relieve nerve pain. These tools may not erase your condition, but they can shift your day from barely getting by to functional.
The Emotional Toll Of Chronic Nerve Pain
This part gets ignored too often. Chronic pain drains energy, patience, and even relationships. Veterans often push through, but there is a cost.
If you notice more irritability, depression, or isolation since your pain began, that is part of the picture. Pain does not stop at your leg or back. It hits your sleep, which hits your mind, which hits your ability to show up for others.
You are allowed to talk about this with your care team. It may even support other connected claims, like insomnia, depression, or anxiety secondary to chronic pain. These can be added as secondary conditions to your primary claim.
Learning From Experts And Other Veterans
You do not have to be your own lawyer and doctor. There are people who spend their lives studying va ratings and helping vets work the system more effectively.
You are never weak for getting structured help with something this technical. It is smart. The system is rules based, and those rules are written in legal and medical language that most people do not read every day.
How Radiculopathy And Sciatica Can Change Your Long Term Plans
Chronic nerve issues shape your future more than most doctors explain in the short visits you get. It may change which work paths are realistic, what retirement looks like, and what you will need as you age.
This is where planning with your full package of veteran benefits in mind is huge. Your ratings today set the foundation for health care coverage, support programs, and family protections down the line.
If you think there is any chance your mobility will worsen, you want that documented early and accurately. You also want to look at legal and financial tools that protect your spouse and kids as years go on.
Sometimes, poor blood circulation issues arise later due to inactivity caused by nerve pain. Keeping a close watch on all symptoms ensures you are ready to file for an increase or new secondary conditions if your health shifts. Having bilateral ratings can also provide a buffer if one side deteriorates faster than the other.
Conclusion
Your nerve pain is real. Your time in uniform and the years since have cost you something that cannot be easily measured. The good news is, VA law actually does give room to recognize radiculopathy, sciatica, and serious nerve pain through the rating system and related programs.
Understanding how VA radiculopathy rating VA sciatica claim nerve pain veteran benefits work does not remove your pain. But it does give you a roadmap for the support you earned. It lets you move from guessing and hoping, to building a claim backed by clear evidence and solid rules.
You are not asking for a handout. You are asking the VA to follow its own standards regarding va claims. With the right records, honest descriptions, and sometimes expert help, you can push for ratings and benefits that match what you live through every single day.


